Isso é porque esses "termómetros" de 10 euros que proliferaram durante o covid não valem nada.
Medições sistemáticas, à mesma distância, dão resultados inconsistentes.
Temperatura corporal de 34-35 graus é hipotermia. Com possíveis consequências graves.
Não se trata de haver ou não impossíveis, trata-se de dados incorrectos.
Para além de serem aparelhos falíveis, estão dependentes de utilizadores não treinados.
Dependem da temperatura ambiente, dependem também, por exemplo, se o sujeito está suado, por exemplo.
Mas o que interessa é que tenhas recuperado bem, isso é que é importante.
Cumprimentos.
"
Experimental protocol
A common user error is
taking a measurement at the incorrect distance from the target.
If the subject’s forehead was visibly moist (perspiration), the NCIT measurement area was dried by blotting gently with a paper towel for 3 min as specified by the instructions for use.
The accuracy of NCIT devices are currently evaluated using the ASTM E1965 and ISO 80601-2-56 standards. Both standards require the laboratory error to be within ± 0.3 °C. Laboratory error measures the temperature against a standardized BBS under controlled conditions and does not include errors introduced by the proprietary software algorithm, user error, physiological variability, and environmental factors. Therefore, in a clinical setting, the variability in the NCIT temperature measurement is expected to be greater than the laboratory error.
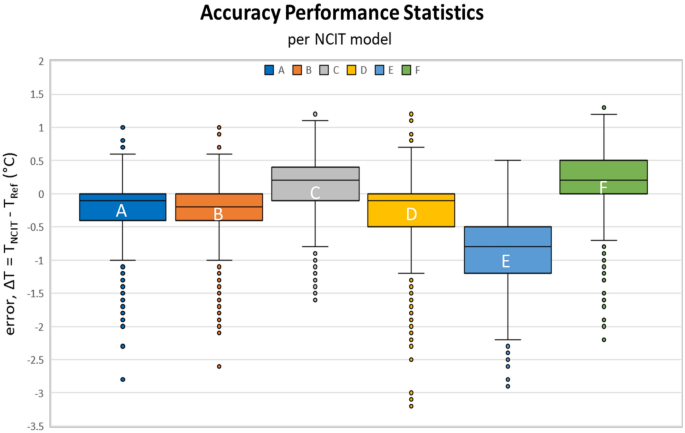
Our study illustrated that the error (ΔT) can range from − 3 to + 2 °C in extreme cases, with the majority of the errors ranging from − 2 to + 1 °C (Figs. 2, 3) outside of the manufacturer’s stated accuracy (Table 3).
Our results showed that the error in the NCIT readings appears to depend upon the subject’s temperature (Fig.
3).
The linear regression of the NCIT measurement error with respect to the subject’s oral temperature for all NCIT models showed a negative slope. As the subjects’ temperatures increase, the NCIT readings transition from overestimating to underestimating the oral temperature.
There are several potential explanations for the negative slope. One possibility is that the reference thermometer was inaccurate. Another possibility is that the offset algorithms used to convert forehead temperature measured by NCIT to oral temperature were inaccurate. Our reference thermometer was calibrated for accuracy across the operating temperatures (Attachment A). Our calibration data showed that the accuracy of the reference thermometer was not dependent on measured temperature. In addition, the reference temperature was obtained using a contact probe (oral) which tends to be more reliable compared to non-contact measurement. Therefore,
our data indicate that the root-cause for this negative slope can likely be attributed to the offset algorithm in the NCITs. Further analysis should be done understand and address the limitations of the existing offset algorithms in the NCITs.
Based on the sensitivity analysis (Fig. 4),
our study showed that some of the NCITs are likely to generate significant false negative readings when used for fever detection. The sensitivity of the NCIT models at 38 °C, the CDC defined temperature threshold1, ranged between 0 and 0.69. Four of the six NCIT models had sensitivity less than 0.5 with two of them below 0.1. Therefore, four of the six models had a false negative rate of more than 50%.
Because of the high probability for producing false negative readings close to the CDC threshold, these NCITs are an unreliable stand-alone temperature screening tool.
"
Non-contact infrared thermometers (NCITs) are being widely used during the COVID-19 pandemic as a temperature-measurement tool for screening and isolating patients in healthcare settings, travelers at ports of entry, and the general public. To understand the accuracy of NCITs, a clinical study...

www.nature.com